Knocked Down, But Not Out: Rainbow Nurse Shares Her COVID-19 Story
Knocked Down, But Not Out: Rainbow Nurse Shares Her COVID-19 Story
by Kenyon Kemnitz

Debbie Faubel has learned to accept that her life won’t look exactly like it did before. She used to enjoy going on long walks, spending hours outside combing around in her garden or flower beds and tackling other projects around the house.
When Debbie joined Rainbow Community Care in 2012 as an Admissions Nurse, she typically worked 10-hour days, often serving as the first contact for patients and families considering hospice care. She evaluated patients to determine their eligibility, provided information, prepared them for admission, and helped manage their medications and equipment needs.
“The best part was helping families get situated to succeed in caring for their loved ones and alleviating a burden off their shoulders,” said Debbie.
“Debbie has this incredible softness to her which makes her an exceptional, well-respected hospice nurse,” said Rainbow Senior Director of Hospice Services Angie Zastrow. “She is relatable and compassionate. When she is listening to you and your story, you really feel a connection. Her presence is calming and brings a sense of peace to the families and patients.”
Debbie thought that she would eventually contract COVID-19. Almost two years after the onset of the pandemic, cases were still on the upswing. It seemed inevitable that no matter how many precautions she took, they wouldn’t be enough to combat the virus forever.
“I was one of the first ones being sent out to go test a patient,” Debbie recalled. “We were all very scared, but we did our best with the knowledge we had. You can’t see viruses, but if that was possible, you would be able to fight against them more effectively. I said, ‘Hey, we’re warriors, we have our personal protective equipment, and we’ll follow the protocols.”
In early December 2021, Debbie was off work for the weekend and started feeling achy and had the chills, but that was a familiar feeling since she often felt cold in the winter. Plus, with her freezer on the fritz, she spent most of her Saturday transporting a bunch of food into a new one so being cold was expected. She took time to rest and curled up with a heating pad but still went about her normal routine, including doing laundry and making a large pot of chili for her church’s upcoming chili dump and Christmas party.
By Sunday, her aches and pains had subsided, and she wasn’t freezing anymore. But later that day after returning home from church, she suddenly felt nauseous, very tired, and experienced what she described as a “yucky, metallic-like” taste in her mouth.
An at-home test kit confirmed she was positive for COVID-19. Debbie made plans to quarantine herself and informed Rainbow of her health status.
“Nothing tasted good at that point,” Debbie said. “I was forcing myself to drink fluids and eat soda crackers and that was pretty much all I could manage.”
That’s when things start to get a little fuzzy for Debbie. She would find herself in different places around the house, not knowing how she got there. Feeling lightheaded, she remembers sitting down and then waking up on the floor in the dining room.
“I was slipping in and out of consciousness and thought, ‘Wow, I’m back in my bed, but this isn’t my bedroom,” Debbie said. “My husband, Todd, came running in and asked me, ‘Do I need to call the ambulance?’”
Debbie knew something wasn’t right. When she started passing out again, she told her husband to take her to the emergency room. The doctors performed a chest X-ray and administered oral steroids. They also gave Debbie a cough suppressant, pain medication, and an inhaler.
“They didn’t want to send me home at first,” Debbie said. “I told them ‘I’m a nurse and I’ll watch myself.’ My oxygen saturation levels (O2 sats) were on the low normal end, so they said, ‘If they drop, then you are right back here in the ER.”
Debbie returned home thinking that getting lots of rest and taking her medications would be enough to combat COVID-19. Four days later though, she got up and became extremely short of breath.
“I checked my O2 sats, and it was down into the 60s,” Debbie said. “I thought I’d open the door and get some fresh air. Well, that didn’t help at all and made me feel worse.”
She immediately called her daughter-in-law, who took her back to the emergency room.
Debbie was hospitalized on December 14th, where another chest x-ray revealed worsening COVID pneumonia. The doctors checked for a possible pulmonary embolism, put her on oxygen, and began telemetry to monitor her heart rhythms. Believing she might have clots in her lungs, they also performed a CT scan.

“There was a heart-to-heart conversation about being intubated and my code status, which was a real awakening and scary moment,” Debbie said.
“Debbie's diagnosis with COVID really "shook" the staff,” Zastrow noted. “It wasn't just the diagnosis since a positive test for staff was not a surprise during this time. It was the severity of her illness that left us grappling with the possibility she may not recover, and we didn't know how to process that.”
Debbie’s CT scan came back negative, but she had severe inflammation in her lungs and body. Every breath she tried to take was a struggle. She wasn’t put on a ventilator because one wasn’t available at the time. BiPAP (Bilevel Positive Airway Pressure) and high-flow oxygen were used to help control her breathing.
“All their respiratory equipment was very limited because they had to share the machines with other patients and myself,” Debbie said. “Both the BiPAP and the high flow oxygen had a different breathing technique, so you had to get used to the change.”

During this time, family members weren’t allowed to stay with patients or visit, so Debbie communicated with her husband and family through text messages asking them to pray for her. She was too weak to talk on the phone.
“I would message him, ‘Good morning, good night, and I love you,’ Debbie said. “Just short and simple stuff. I thought I was young and healthy and would get COVID, but never imagined I’d end up in the hospital.”
It was during this time that Debbie discovered that her older cousin, David Graff, had also been hospitalized with COVID at Aurora Summit. She remembers sending him some encouraging messages but doesn’t know if he ever saw them.
“I told him it’s going to be rough, but you have to fight like hell,” Debbie said.
Unfortunately, her cousin was placed on a ventilator and never came off the device. He passed away a few days later.
Debbie was also facing the fight of her life. One day she wasn’t able to contact her husband at all. He became worried and called the hospital.
“It sounded like it was touch and go there for a little bit because they said I was in a pretty deteriorated state,” Debbie said. “Even some of the staff I knew from working at Marquardt for over 21 years, requested to be reassigned to different patients because they couldn’t handle seeing me like that and continue to provide the hands-on care that was needed.”
Co-workers at Rainbow learned about Debbie's condition during this time and wanted to help but were unsure how.
“It was very difficult for everyone,” Zastrow said. “There were feelings of helplessness throughout the organization. They all wanted to rally around Debbie and support her, but there was simply nothing they could do.”

Debbie thinks what finally helped her recover was when they were able to leave her on the BiPAP continuously for almost 24 hours. But any time she moved or turned in bed, it would trigger a coughing episode and shortness of breath, and it would take her some time to recover.
“You could feel the fluid shifting from one side of the lung to the other and it would take about 20 to 30 minutes for me to recover and my oxygen saturation, heart rate, and blood pressure to get back to normal,” Debbie said.
After spending nearly her entire career as a nurse helping others, it was difficult for Debbie to go from being a caregiver to a patient.
She credits the staff at Watertown Regional Medical Center for taking such great care of her during an unpredictable and stressful time.
“I entrusted my body to them and the care I received was great,” Debbie said. “The staff went above and beyond the call of duty. They would sit vigil at my bedside and hold my hand or just sit quietly until my breathing was somewhat managed. Administrative staff even came in to bring me tissues, and mouth swabs or to fill up my water and help out the nursing staff who were overwhelmed.”

Debbie has vague memories of her time in the hospital, but she recalls a surreal experience of being in total darkness and feeling like she was in another realm.
“It felt like being in a black space filled with tar or a shiny garbage bag and as I breathed it was moving with me,” Debbie said. “I wasn’t afraid. There was nobody there, just absolute quietness and peace. I was looking for the light but never found it. When I woke up, I knew it wasn’t my time to die and that I had to give it my all to recover.”
After eight days, Debbie was finally discharged on eight liters of oxygen. She could reduce it to four liters while resting but needed eight liters with any type of activity. Debbie knew she needed medical equipment to aid in her recovery.
“I was focused on getting back home so I could still be functional,” Debbie said. “I was really worried I would be sent to a nursing home for rehab since I was pretty debilitated. When I got home, it took me half an hour to climb just seven steps to our main floor.”
Still weak and having lost significant muscle strength from being bedbound in the hospital, Debbie faced a challenging road ahead.

The Watertown-Beaver Dam Elks Lodge No. 666 delivered a shower bench, wheelchair, commode, and walker the day after she arrived home, ensuring she had everything she needed before Christmas.
“I used the commode and wheelchair very little since we had chairs set up every few feet to the bathroom,” Debbie said. “There was no way we could have gone out to purchase all that equipment because it would have been incredibly time-consuming.”
Before the new year, Marquardt Home Health provided physical therapy and nursing services sessions at Debbie’s home. But with her insurance restarting at the beginning of the calendar year, it was determined it would be more cost-effective to leave Debbie with recommendations and exercises she could do on her own to help her regain her strength.
“There were days I slept a lot, but when I was awake, I would walk a little here and there,” Debbie said. “I followed their guidelines and did little circles around the kitchen, or living room to get some walking in and then up and down the hallway. It was challenging, tiring, and fatiguing.”
Debbie has been on a long road to recovery, but that journey has been anything but easy. At times, it felt like she would take one step forward only to take two steps back.
Her hair started falling out and became very thin. She would find huge clumps all around the house or in her hairbrush. More tests and lab work were ordered to see if it was related to her thyroid. But it turned out it was related to the extreme stress of her situation.
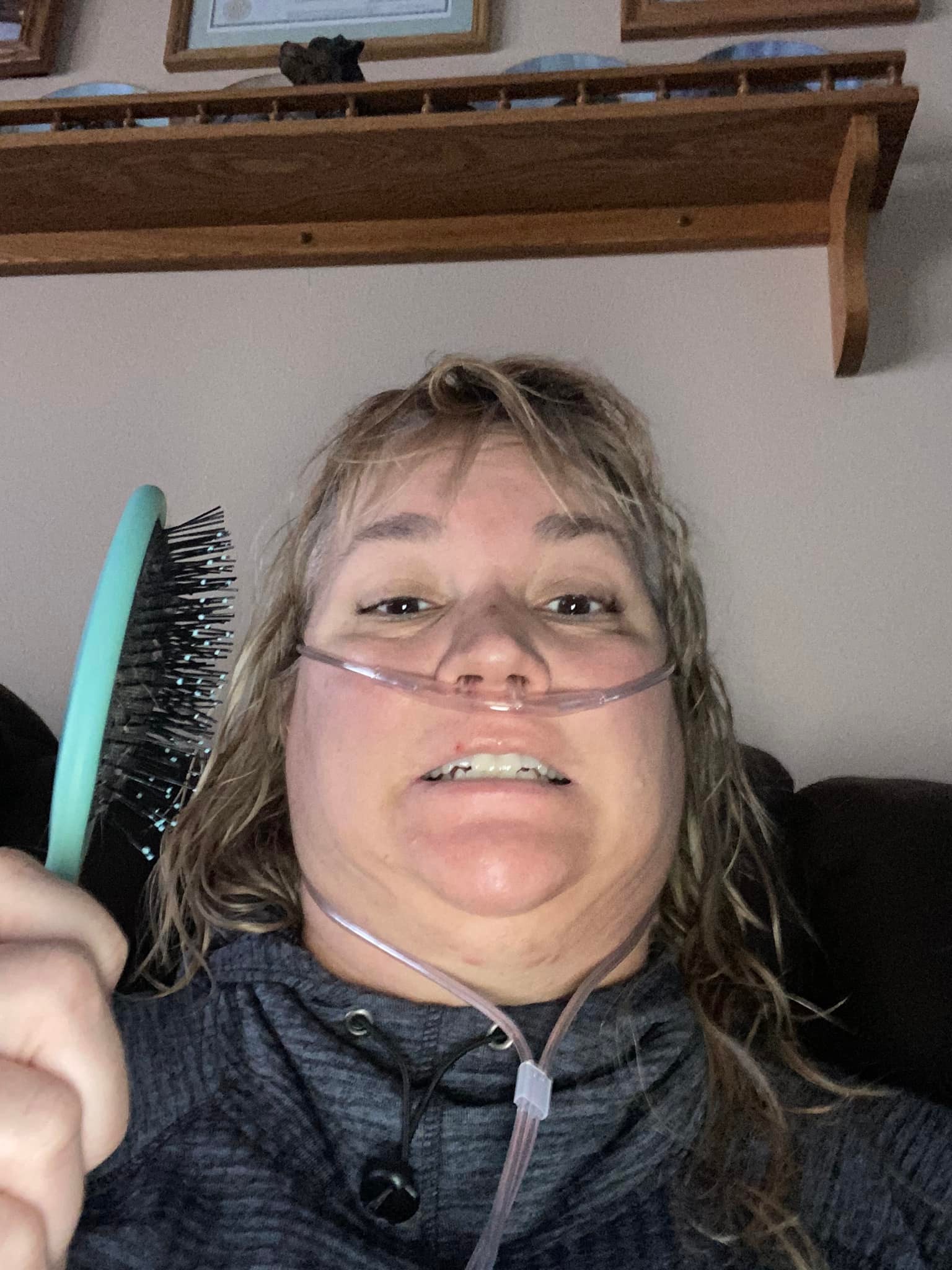
“It felt like I had a deep cut or had been hit over the head,” Debbie said. “I couldn’t touch it, and my hair was everywhere, getting stuck and wound up tight in the vacuum cleaner. I got it cut short and didn’t use any heat or hair coloring.”
Learning to be patient was essential and not trying to do too much too quickly. For a while, Debbie needed help getting in and out of the shower and getting dressed. Gradually, her hair started to grow back.
“My strength wasn’t coming back as fast as I wanted. I was only doing stairs when my husband was home and that was a challenge in the beginning. I had a goal to get down to the basement because I didn’t want him to do the laundry,” Debbie laughed.

When her husband returned to work after the holidays, Debbie had both of her daughters-in-law on standby if she needed them. Her brother would also stop by on his way home from work in the afternoon to let her dogs out. What had been normal daily activities were now tasks she couldn’t perform on her own.
Debbie also worried about her job status due to the time she had missed from work, but Rainbow assured her that her job wasn’t in jeopardy.
“The thought of her not returning to the bedside was just crushing,” Zastrow said. “But she needed to focus on her health knowing we would support her any way we could once she was ready. We understood she might not come back in full capacity, but we looked forward to her returning in some way.”

Debbie started to see more improvement even if it wasn’t coming as fast as she would have liked. A couple months later, she was able to drive while using oxygen, even with the bulky tank along for the ride. Debbie attended pulmonary rehab from February through March and had numerous visits to see a cardiologist, pulmonologist, and neurologist. Finally, she was taken off the oxygen in the middle of May. Debbie also needed to see an Ear, Nose, and Throat (ENT) specialist, a speech therapist, and an occupational therapist. The medical treatment used to combat the virus also affected her vision, causing cataracts, stabbing eye pain, and dental issues.
Debbie still experiences Post-Traumatic Stress Disorder (PTSD) from all the beeping alarms in the hospital and suffers from brain fog and short-term memory loss. Those challenges cause her to forget certain things and lead to difficulty concentrating.
“I get distracted easily now, and I was never like that,” Debbie said. “I have to write down a lot of things, set reminders on my phone, and keep tons of notes at home. I feel like I’ve aged about 20 years and so has my brain.”
Debbie continues to experience the effects of long-haul COVID and is uncertain what that means for her health down the road.
“I still have shortness of breath if I’m up or doing something too long and I get really lightheaded,” Debbie said. “My coughing has improved but I have to keep water with me and carry a larger purse with an inhaler just in case.”
Debbie has been diagnosed with Postural Orthostatic Tachycardia Syndrome (POTS), a condition where the heart rate increases abnormally when a person stands up, causing symptoms like lightheadedness, dizziness, and fatigue. She also experiences frequent headaches.
“They don’t know if I will fully recover, because with this virus, nobody knows,” Debbie said. “I have come to accept my limitations and look at what I still have rather than what I have lost. I use humor a lot.”
Debbie knows when she needs to rest and how much she can realistically accomplish before extreme fatigue takes over.
“I have to look at what I need to accomplish for the day, break it down into smaller tasks, and take frequent rest periods because fatigue can come on very suddenly out of nowhere,” Debbie explained.
She remains cautious about having her family nearby when she leaves the house, especially for walks. Places that have a lot of hills, like the Milwaukee Zoo, are now off-limits for her.
“I used to go on five-mile walks but now my average is probably about mile, and I can’t go alone either,” Debbie said. “You look at the situation and determine how much you can do.”
Debbie is still grateful she can enjoy life once again. She has come to appreciate some simple pleasures like watching how many birds visit the feeders outside her house. She still gardens and plants flowers, but on a much smaller scale. Despite many challenges, Debbie has adjusted and after almost a year way, was able to return to work in November 2022, but in a different role.
 While recovering, Debbie looked forward to the days when her two sons and grandchildren could come over to visit.
While recovering, Debbie looked forward to the days when her two sons and grandchildren could come over to visit.
“Taking a phone call and maneuvering through a patient’s chart was difficult for me if I didn’t do it often enough,” Debbie said. “When I came back, I knew physically I couldn’t return to my old role. I just needed a sense of belonging and finding out where I could be the most useful to my team.”
Debbie has now embraced her role as a clinical assistant in palliative care either at home or at the Rainbow Hospice Care Inpatient Center two days a week for four hours and picks up a few extra hours if needed.
“They’ve trained me on how to pull medical records, and which documents we need for an admission,” Faubel said. “I’ve also been helping with updating medications into the patient’s charts.”
“Debbie has not had it easy,” Zastrow said. “She never did return to her baseline health but was able to rejoin Rainbow in a new position, surrounded by those who care deeply for her. That is something we are all incredibly thankful for.”
As she approaches the four-year anniversary of her COVID diagnosis, reflecting on pictures from when she was in such a vulnerable state is difficult for Debbie.
 Debbie and her husband, Todd, during Christmas 2023.
Debbie and her husband, Todd, during Christmas 2023.
“I still wonder why it took so long to begin to heal and why I still experience these long-lasting effects,” Debbie said. “I see a body that was extremely ill, and know I was one of the lucky ones. There were times when I wondered if I was going to get better. Would I need to call hospice? It is a longer recovery than you’re prepared for, but I knew what I needed to do and to keep pushing forward.”
Debbie faced her situation head-on, took charge of her recovery, and persevered despite a few setbacks.
“I think my situation changed many minds about the virus, proving it was very real and not a hoax after I shared what had happened to me,” Debbie stated. “My faith, family, friends, and positive attitude helped me get through everything. COVID strengthened my faith, and I gained a perspective to appreciate all the blessings God has given me.”
